Over the last several months, we have been faced with many challenges associated with COVID-19. Our elders are the highest at risk. As a result, long term care is experiencing a time of trials never seen before. Consequently, a high percentage of our elders are losing weight associated with COVID-19 (may be from the acute illness or unintended consequences of the guidelines to keep them safe- i.e. isolation/depression).
A team approach to assessment, prevention and intervention is necessary to support the best outcomes possible.
Before going any further, I want to discuss the personal implications of food. Think about your most “favorite food”, how does it taste? Why does it bring you enjoyment? Would you prefer a liquid oral supplement over that? I doubt it. NOW, think about a time when you were very ill, at this time, could you eat even your most “favorite food”? Maybe not. What did you do? These are the times we are most at risk for weight loss and associated problems that may follow; dehydration, muscle wasting, pressure injuries, etc. Food is incredibly personal. We associate food with family memories, holidays, social settings. We nurture our children with food; bring others joy with cooking. We receive comfort from food and give love with food. If we are not aware of what our elders love to eat, we have failed before we even begin to try and help! This is why food must always be considered FIRST.
ASSESSMENT:
Your Interdisciplinary Team is essential to determine the best plan of care. Utilize your Registered Dietitian who is educated and trained to assess areas related to nutrition care. Include first-line staff as a part of your team when discussing nutritional status. First-line staff such as Certified Nursing Assistants and Dietary Aides can offer valuable information regarding resident’s food preferences, intake and can often offer creative and common-sense interventions.
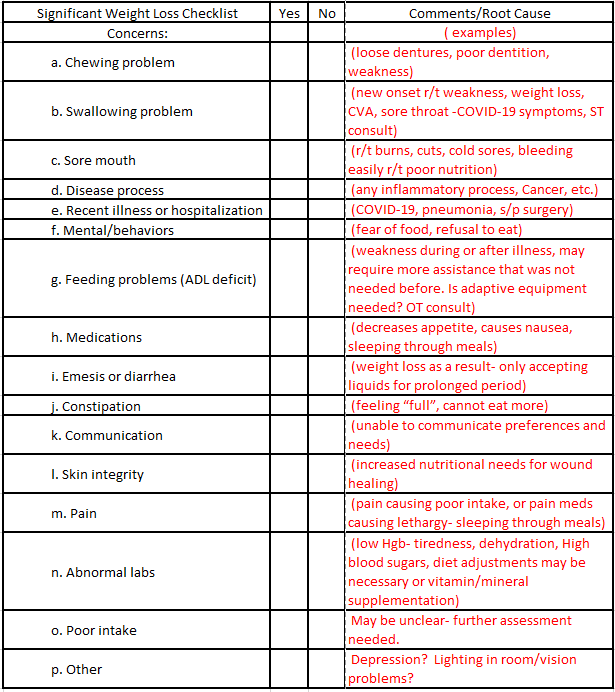
Below is an example of a simple checklist that may be used to identify the root cause of weight loss.
PREVENTION:
**A good initial assessment and visit/interview with the resident is important:**
Food Preferences- send foods well liked, provide alternatives for dislikes.
- Food Preferences- send foods well liked, provide alternatives for dislikes.
- Is there a history of weight loss or poor intake? What have they done as an intervention or was weight loss intentional?
- Observe and ask about ADL(Activities of Daily Living) concerns: “Do you need assistance with meals?”, “Would you like help to cut your meat?”
- Observe and ask about chewing or swallowing difficulty.
- Does the resident follow a therapeutic diet at home? Does their current diet need to be liberalized to promote better meal intake?
- Any recent or chronic constipation, nausea, vomiting or diarrhea?
**Practices to promote nutritional status and hydration:**
- Provide meals that meet nutritional needs (adequate protein, calories, micronutrients). Adjust diet to meet nutritional needs.
- Provide at least 2 glasses of fluid at each meal to encourage hydration.
- Offer snacks with fluids between meals. Have snacks available for residents with special needs (i.e. puree diet, diabetic, etc.).
- Plan food related activities on a regular basis.
- Improve food and beverage choices. Implement select menus and more than one meal alternative.
- Visit residents on a regular basis (at least quarterly), update preferences and observe for any changes (i.e. requiring more assistance, etc.).
- Think “out of the box”. What fun ideas can you include to promote enjoyment of food?
- Ice cream “truck”- serve “old time” novelty favorites; push up pops, ice cream sandwiches, novelty ice cream bars. Simple frozen ice can increase hydration.
- Prepare recipes provided by residents. Ask them to share their favorite recipes! Include the item in your menu or for a special occasion (example: “Miss Millie’s Fried Chicken”).
- Include holiday and event meals planned by the residents.
- Theme day meals.
- Homemade milkshakes can increase calories, protein and fluid intake.
- Foods and smells that bring back memories: Hot dogs at the ballpark, bread baking in the oven, turkey roasting in the oven, etc.
INTERVENTION:
Level 1:
- Update food preferences- offer foods that he/she likes.
- Liberalize diet (d/c therapeutic restrictions).
- Consider high calorie snacks between meals- start QD.
- Consider additional food w/ meals only if resident is eating 100% already (large portions, extra desserts, milk, entrees).
- Fortified foods with meals (plan a rotating schedule to prevent taste fatigue).
- Consider consistency changes if appropriate.
- Ask family to bring in favorite homemade foods.
Level II:
If food interventions are not working and nutritional requirements are elevated to the point resident is unable to take in adequate nutrition with meals/snacks (i.e. multiple pressure sores, end stage COPD)
- Utilize a high calorie/protein supplements, offer several options/flavors.
- Determine acceptance of supplements prior to ordering (visit resident w/ supplement and observe acceptance). Document if resident refuses or dislikes.
- Always give liquid supplements between meals.
Level III:
- Current literature indicates that enteral feedings should not be used for dementia residents. Instead, hand feeding and encouragement are still recommended.
- Appetite stimulant drugs have significant side effects in elderly residents. If ordered, please consider x 30 day auto-stop and evaluate effectiveness.
- Consider Hospice if weight loss continues despite interventions over a prolonged period.

